Hip Conditions & Treatments
There are a wide range of conditions that can result in hip pain, these include:
- Hip Arthritis
- Hip Bursitis
- Femoro-Acetabular Impingement
- Avascular Necrosis of the Femoral Head (AVN)

Hip Arthritis
The role of the cartilage in the hip, just like in any other joint, is to provide a smooth gliding surface of this ball and socket joint.
Osteoarthritis occurs when the cartilage that surrounds the femoral head and lines the acetabular cup gradually breaks down, thins out and wears off leaving the bones exposed. This condition is also called “wear and tear”. During this process spurs and cysts form and the ball and socket deforms, becomes incongruent, causing friction. The cartilage particles (debris) irritate the joint lining resulting in inflammation.
There is another type of arthritis, called inflammatory arthritis, when the inflammation is the primary cause and cartilage breakdown is the secondary process. There are several types of inflammatory arthritis including; rheumatoid arthritis, gout, psoriatic arthritis and ankylosing spondylitis.
- Hip Pain, typically at the front (groin) and side of the hip.
- Reduction in mobility, limp
- Stiffness of the joint, reduced range of motion
Non-surgical
- Weight Loss – It has been demonstrated by scientific studies that excess body weight is associated with increased symptoms of arthritis and weight-loss has beneficial effects on symptoms caused by arthritis.
- Amending lifestyle, e.g. moving from high intensity training to lighter activity such as cycling or swimming
- Rest or temporarily reducing aggravating activities
- Use of assistive devices such as walking sticks
- Simple pain medication
- Anti-inflammatory treatment
- Non-steroidal anti-inflammatory medication
- Steroid injection into the hip joint (usually performed by CT or US guidance)
Surgical
- Total Hip Replacement
Hip Bursitis
Bursae are cushion like sacs filled with small amounts of fluid, these are present in between the bone and soft tissue located within and around the hip joints. Their role is to reduce the level of friction that occurs during physical movement. Bursitis occurs when these sacs become irritated and inflamed.
- Pain or tenderness in the outer hip region, or in the groin. As time progresses the pain may travel down the thigh and sometimes in the buttocks becoming a dull ache
- Swelling is usually minimal at the hip joint
- Limp due to pain and weakness from a lack of muscle action
- Difficulty sleeping on the effected side due to the tenderness over the bony prominence of the hip
- Initially rest and temporarily avoiding overuse and aggravating activities
- Anti-inflammatory Medication
- Steroid injections
- Physiotherapy including stretching the tight fascia over the bony prominence and strengthening the hip muscles to reduce pressure and friction on the bursa
Fermoro-Acetabular Impingement (FAI)
Impingement of the hip joint occurs when bony overgrowth, called bone spurs develop around the femoral head and/or along the acetabulum causing abnormal contact between the hip bones. FAI prevents the structures from moving smoothly during activity. Over time, this can result in tears of the labrum (a fibrous ring around the rim of the acetabular cup) and a breakdown of articular cartilage (osteoarthritis). Friction then occurs resulting in pain and restricted motion.
- Discomfort with increased physical activity, in particular movements that come from the hip such as sitting or standing.
- An inability to bend the hip beyond a 90 degree angle without sharp pain in the groin.
Non-surgical
- Symptomatic pain and anti-inflammatory medications
- Rest and avoiding painful positions and activities of the hip joint
Surgical
- In early stages, before arthritis starts developing a hip arthroscopy may provide symptomatic relieve by removing bony prominences and repairing labral tears, however long-term benefits are yet to be scientifically proven
- In later stages, when arthritis has developed hip joint replacement may be indicated
Avascular Necrosis of the Femoral Head
Avascular Necrosis (AVN) occurs when the bone tissue of the femoral head begins to breakdown due to a lack of blood supply to the area. The cause of this restricted blood flow is mostly unknown. The bone slowly softens and collapses causing significant pain, stiffness and often disability.
- Discomfort or pain in the hip joint, usually in the groin
- A feeling of stiffness, locking, clicking or catching in the hip
- Noticeable decrease in hip motion and rotation
Non-surgical
- Symptomatic pain and anti-inflammatory medications
- Rest and off-loading the hip using crutches
- Bisphosphonates, medication used for osteoporosis to prevent bone loss
Surgical
- Core decompression. The affected bone segment is perforated to release the venous pressure in the femoral head and to encourage blood flow and healing. This procedure is only effective at an early stage before the affected segment of bone collapses
- This is a surgical procedure of realigning and rotating the effected femoral head segment out of the weight-bearing zone
- Hip joint replacement may be considered in the later stages when the avascular femoral head segment collapsed, and arthritis has developed
Total Hip Replacement
During total joint replacement surgery, the damaged cartilage is replaced by artificial surfaces. Joint replacement surgery for hip and knee arthritis is one of the most common and most successful orthopaedic procedures in terms of improving quality of life.
The patients who benefit the most from this surgery are the ones suffering from end stage of this condition, when non-operative treatment is no longer able to control their symptoms, when their pain and disability interferes with their daily activities and impairs their quality of life. Making the decision regarding whether you are at the appropriate stage to benefit from a joint replacement or not, needs a very delicate and balanced consideration of your individual circumstances and condition, and our experienced team ensure that we provide you with all of the necessary information and guidance to assist you to make the right choice for you.
Considering the extent of the operation patients endure significant discomfort (pain, swelling, bruising) in the early post-operative period. There are many aspects of the surgical procedure and post-operative care which aims to reduce the risks of discomfort and optimise the recovery period. An active and complex pain management is employed; blood clot prevention and early mobilisation within hours following surgery are also part of the treatment regime to make the recovery as painless and comfortable as possible.
Longevity of the prosthesis is a crucial question. According to laboratory studies the advanced materials used in hip replacements are able to withstand mechanical wear equivalent to 20-30 years of use in the human body. The wear happens between the bearing surfaces. Although the ceramic on ceramic bearing surface theoretically provides the least wear, advances in manufacturing plastic linings during the last 10 years have halved the revision rate and have virtually eliminated the “polyethylene disease”, bone resorption and prosthetic loosening caused by tiny debris from the plastic component. The most suitable prosthesis for you will be discussed and selected at the time of your consultation.
The most common and well established “traditional” surgical technique is the posterior approach, which provides reliable results.
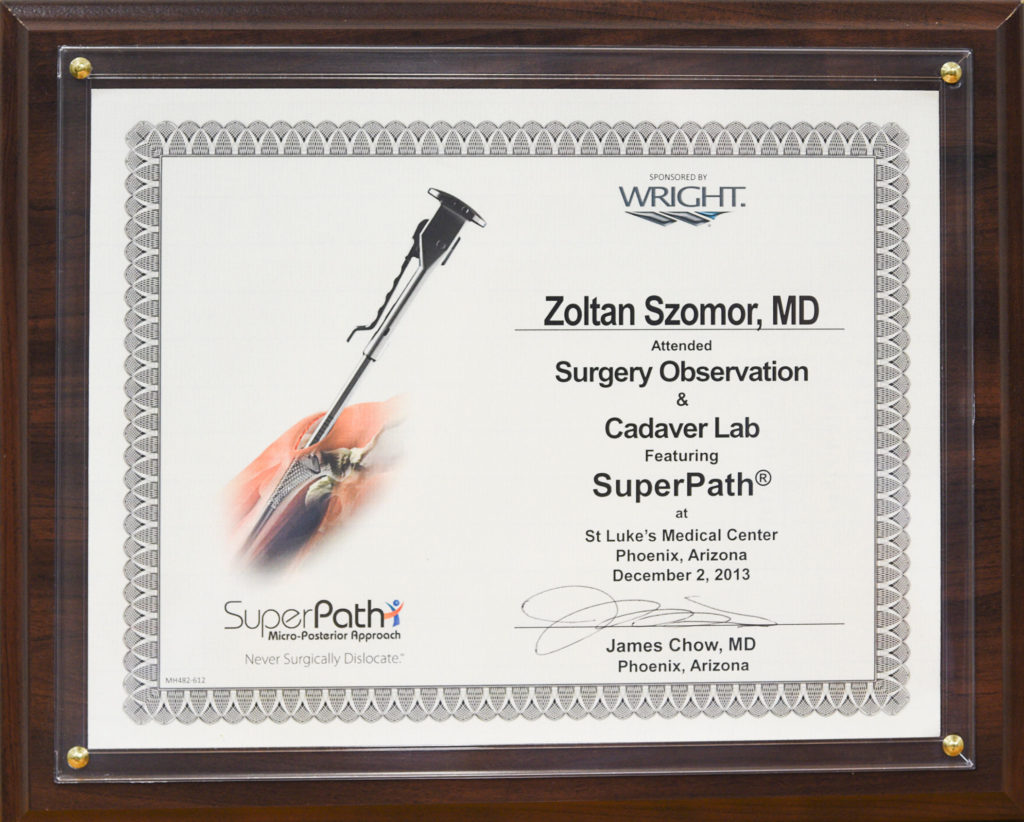
In recent years significant efforts were placed towards developing minimally invasive, tissue sparing surgical techniques to perform total hip replacements. These include the anterior (front) approach, as well the superior (side) approach, called the SuperPATH. I have been using the SuperPATH technique since 2013 and was one of the first surgeons introducing this technique in Australia. This surgical approach utilises the upper (superior) third of the incision used for the posterior approach. Through this small incision the femoral neck is resected without the hip being dislocated, while the acetabular (cup side) preparation is done though a percutaneous cannula, thereby minimising any soft tissue injury.
However, the most important aspect of any successful joint replacement is the surgeon’s experience and being able to implant the prosthesis in the correct position regardless of the surgical technique. As an experienced surgeon I am familiar with all available surgical options and select the most appropriate one for my patients, one which works best for the individual patient. The most suitable surgical approach will be discussed and selected at the time of your appointment.
Revision Hip Replacement
What is a Revision Hip Replacement?
If a hip replacement fails for any reason, for example through prosthesis wear, loosening, bone resorption, infection, injury, peri-prosthetic fracture or any other cause, then it may be necessary to remove and replace it with a new prosthesis. This procedure is called a revision surgery.
A revision hip replacement is a more complex procedure which usually requires special prosthetic implants supplementing weak or missing bony or soft tissue structures. According to the 2017 Australian National Joint Replacement Registry’s report at 10 years the total hip replacement revision rate was around 5.1%, and at 15 years it was 8.1%.
SuperPATH Hip Replacement
A SuperPath® Hip Replacement is designed to precisely reconstruct the hip without cutting critical tendons and stretching or traumatising muscles that are important to hip function (MicroPort Orthopaedics, 2017). Using this minimally-invasive, tissue-sparing surgical technique for total hip replacement, because of the elimination of damage to important structures surrounding the hip during surgery, patients typically have a short hospital stay and most patients able to walk the same day as their surgery (MicroPort Orthopaedics, 2017). If SuperPath treatment is appropriate for you, this is will be discussed in further at time of consultation.
Disclaimer: Individual results and activity levels after surgery vary and depend on many factors including age, weight and prior activity level. There are risks and recovery times associated with surgery and there are certain individuals who should not undergo surgery.